Cost of Autism Stem Cell Therapy at a Glance
Families often ask how much is stem cell therapy for autism, and the answer depends on many moving parts. Most centers quote between $10,000 and $40,000 per treatment cycle. That range includes pre-treatment diagnostics, laboratory preparation of cells, the infusion itself, and initial follow-up visits. Higher costs usually reflect more specialized cell types, deeper laboratory quality checks, or bundled rehabilitation programs.
At Liv Hospital and elsewhere, the total price most depends on which stem cell line you use—mesenchymal stem cells for ASD are the most common—how many doses your child receives, and whether the protocol includes inpatient stays or anesthesia. Families also spend on travel, lodging, and post-infusion behavioral and speech therapy integration. Understanding what drives each cost helps you compare quotes and build a realistic budget.
What Drives the Price: Comprehensive Cost Breakdown
Pre-treatment evaluation and diagnostics: Before any infusion, clinics run neurology panels, pediatric assessments, immunology labs, MRI or EEG scans, and standardized ASD behavior scales. These tests identify eligibility and guide dosing. Expect $1,500 to $4,000 for this workup, depending on imaging depth and specialist time.
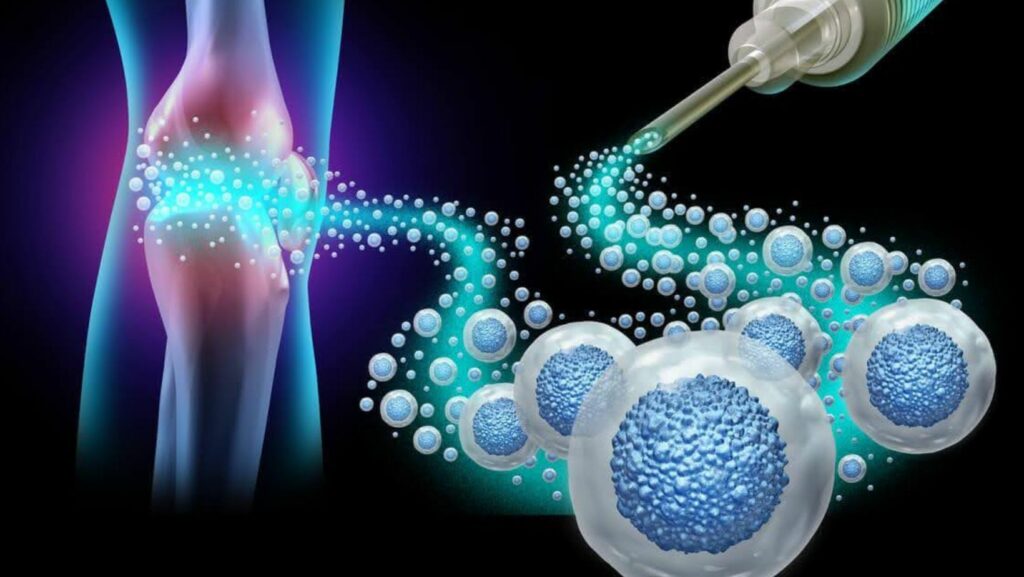
Cell sourcing and lab processing: Most protocols rely on mesenchymal stem cells harvested from bone marrow or umbilical cord tissue. Neural stem cells and hematopoietic stem cells may be used in select cases. Lab teams must culture, expand, and verify each batch under GMP-grade conditions. Quality control checks—viability, sterility, potency—add $3,000 to $12,000 per batch, with higher prices for autologous harvest and custom dosing.
Administration method and setting: Intravenous stem cell infusion is the standard route, delivered in an outpatient suite or day clinic. Intrathecal injections—cells delivered into spinal fluid—cost more because they need anesthesia, operating room time, and longer monitoring. Inpatient observation can add $500 to $3,000 per night if your child needs overnight care.
Post-treatment services: Gains emerge faster when families follow infusion with pediatric rehabilitation, speech therapy, and occupational sessions. Liv Hospital’s multidisciplinary program includes follow-up visits, telehealth check-ins, and home-program guides. Budget $100 to $300 per session; packages may discount bulk hours.
What’s Included at Liv Hospital: Multidisciplinary Program Value
Interdisciplinary oversight: Liv Hospital coordinates neurology, pediatrics, immunology, and rehabilitation specialists from the first evaluation through aftercare. Weekly team meetings review your child’s progress, adjust dosing or cell type, and solve any safety concerns. This oversight catches adverse events early and tailors the protocol to your child’s evolving needs.
Individualized protocols and cell types: Some children respond best to mesenchymal stem cells; others benefit from neural stem cells or a combination with hematopoietic lines. Liv Hospital’s team designs the cycle count, infusion schedule, and dose based on age, symptom severity, and inflammation markers. One child might need a single high-dose infusion; another could receive smaller doses spaced over three months.
Safety, ethics, and quality: Every family signs detailed informed consent forms that explain risks, expected benefits, and research status. Cells undergo sterile processing in accredited laboratories, and adverse event monitoring continues through six-month follow-up. Liv Hospital collaborates with research institutions to share anonymized data, advancing clinical evidence for stem cells in ASD while protecting patient privacy.
Typical Price Ranges and International Comparison
For budgeting your treatment, it helps to know the usual per-cycle range in Turkey at Liv Hospital is approximately $15,000 to $25,000, and that figure typically includes initial diagnostics, cell preparation, one intravenous infusion, and three months of follow-up visits. Additional cycles, intrathecal delivery, or extended inpatient stays push totals higher. The package covers tests like MRI and immune panels, but families arrange their own travel and lodging.
How prices compare in Turkey versus the United States, Mexico, India, and other destinations reveals wide gaps. U.S. clinics often charge $30,000 to $50,000 per cycle because of higher labor and compliance costs. Mexico and India quote $8,000 to $20,000 but may offer less integrated rehabilitation. Turkey strikes a middle ground: advanced laboratory standards, experienced specialists, and reasonable pricing. When evaluating cost-to-value, ask what rehabilitation services, safety monitoring, and follow-up care are bundled rather than focusing on the infusion price alone.
Evidence, Expected Benefits, and Realistic Outcomes
Improvements that parents and clinicians report include better social communication—more eye contact, longer conversations—enhanced attention spans during tasks, clearer language development, and reduced repetitive behaviors like hand-flapping or echolalia. Some children sleep more soundly or show less irritability. What remains uncertain is how durable these gains are, which children respond best, and whether cells truly regenerate damaged neural circuits or simply reduce neuroinflammation in autism temporarily.
Autism stem cell therapy is not a cure. It is a supportive intervention that may improve function in some individuals. Clinical evidence for regenerative medicine for autism comes mostly from small, open-label trials; larger randomized controlled studies are underway but incomplete. Families should weigh promising case reports against the lack of regulatory approval in most countries and the reality that outcomes vary widely.
How Liv Hospital’s Approach Impacts Cost and Outcomes
Targeting neuroinflammation in autism and supporting neural regeneration drives Liv Hospital’s protocol design. The team believes many ASD symptoms arise from immune dysregulation and poor neural connectivity. Mesenchymal stem cells secrete anti-inflammatory molecules, improve oxygen delivery, and may prompt the brain to repair damaged pathways. Dosing, timing, and cell source are chosen to maximize these mechanisms while minimizing side effects.
Structured post-treatment rehabilitation reinforces gains by building new skills during the window when brain plasticity peaks. Behavioral therapy teaches social routines, speech therapy strengthens language circuits, and occupational therapy addresses sensory sensitivities. Liv Hospital’s program assigns dedicated therapists who track milestones and adjust exercises weekly, ensuring the biological boost from stem cells translates into real-world progress.
Step-by-Step Pathway and Timeline
Before scheduling an evaluation: Submit your child’s medical records—previous ASD assessments, behavior scales, blood work, imaging—through a secure portal. A Liv Hospital coordinator and physician review eligibility via teleconsult, explain the protocol, answer questions, and provide a preliminary cost estimate. This stage takes one to two weeks.
Treatment day: You arrive at the clinic for final blood draws and vital signs. Lab technicians thaw or prepare the stem cell dose under sterile conditions. A nurse starts an IV line, and the infusion runs over thirty to ninety minutes. Monitoring continues for two hours post-infusion. Most children go home the same day; a few stay overnight if they received intrathecal administration or showed minor reactions.
Aftercare: Follow-up assessments occur at one week, one month, three months, and six months. Therapists measure behavior scales, language milestones, and parent-reported quality of life. Home programs include exercises, sensory activities, and diet recommendations. Remote support from the Liv Hospital stem cell program team is available via video call or messaging, allowing families anywhere to stay connected.
Budget Planning: Sample Scenarios, Add-ons, and Hidden Costs
Sample budgets: A one-cycle plan with umbilical-cord mesenchymal stem cells, outpatient IV infusion, and three months of rehab might total $18,000. A two-cycle plan using autologous bone-marrow cells, intrathecal delivery, one overnight stay, and six months of therapy could reach $35,000. The subtotal changes when you choose higher-potency cell lines, add imaging between cycles, or request in-home therapy visits.
Travel and logistics for Turkey: Round-trip flights for parent and child from North America run $800 to $1,500; from Europe, $200 to $600. Turkish e-visas cost about $50. Budget $60 to $120 per night for mid-range lodging near the hospital, plus meals, local transport, and translation services if you don’t speak English or Turkish. Total travel and lodging for a two-week stay averages $2,000 to $4,000.
Payment options: Liv Hospital accepts deposits by wire transfer or credit card, with the balance due before infusion. Some families use health savings accounts or flexible spending accounts if their plan allows experimental treatments. International wire fees add $30 to $75. A few U.S. tax advisers help document autism stem cell therapy as a deductible medical expense. Charitable grants for ASD treatments are rare but worth researching through autism advocacy groups.
Questions to ask any clinic: Request itemized quotes showing diagnostics, cell dose and viability, number of infusions, included rehab hours, and follow-up schedule. Ask about refund policies if treatment is postponed and whether prices are guaranteed in writing.
Insurance, Regulation, and Ethics: What Families Should Know
Coverage realities are blunt: most insurers deny autism stem cell therapy, labeling it experimental or investigational. To appeal, document medical necessity with letters from your pediatrician and neurologist, peer-reviewed studies showing potential benefit, and proof that conventional therapies have plateaued. Even strong appeals rarely succeed, so plan to self-pay and pursue reimbursement afterward.
Regulatory status varies by country. Turkey allows stem cell use under Ministry of Health oversight; the U.S. FDA has not approved stem cells for ASD outside clinical trials. Informed consent forms at reputable clinics explain this regulatory gap. Liv Hospital shares anonymized treatment data with research institutions to build the evidence base, and safety monitoring includes tracking any adverse events through national registries.
How to Compare Quotes Apples-to-Apples
Checklist: Verify that each quote lists the exact tests included—MRI, immune panels, behavior scales—the stem cell dose in millions of cells, viability percentage, number of infusions, hours of rehabilitation per week, and how many follow-up visits or teleconsults are covered. Ask whether the price locks in exchange rates if you’re paying in a foreign currency.
Outcome tracking: Baseline and post-treatment metrics that indicate value beyond price include standardized ASD severity scales (CARS, ADOS), parent-reported quality-of-life surveys, speech-language assessments, and video recordings of social interactions. Clinics that track these systematically and share aggregated results demonstrate accountability and help you measure whether the investment delivered meaningful change.
Frequently Asked Questions
How many cycles are typical, and how far apart? Most protocols start with one or two cycles spaced three to six months apart. Some children show gains after a single infusion; others benefit from a second dose.
Are donor cells or autologous cells used, and does that affect cost? Donor umbilical-cord cells are more common and cost less than autologous bone-marrow harvest, which requires surgery and longer lab time.
Is intravenous stem cell infusion enough, or is intrathecal needed? IV delivery works for many children. Intrathecal may be considered if neuroinflammation is severe or prior IV cycles showed limited benefit.
What ages are eligible for autism stem cell therapy at Liv Hospital? Most programs accept children aged two to eighteen. Adults may qualify if evaluation shows active neuroinflammation and realistic goals.
How soon might changes be observed, and how are they measured? Some families notice shifts in attention or sleep within weeks; language and social gains emerge over two to six months. Progress is tracked with behavior scales and therapy notes.Can we continue therapies at home, and does Liv Hospital coordinate with local providers? Yes. The hospital shares treatment summaries and home-program guides with your local speech, occupational, and behavioral therapists to ensure continuity of care.